- Created by Bridget Fritzke, last modified on Aug 19, 2014
You are viewing an old version of this page. View the current version.
Compare with Current View Page History
« Previous Version 15 Next »
Submitting HCFA 1500 claims electronically
After generating a HCFA 1500 form, adjust the claim form as needed using the SHOW FORM DATA button.
Each field name has a corresponding value. Double-click in the value field to update the field, click out of the cell to save the change, and click Update.- Click SUBMIT ELECTRONICALLY.
- If more than one insurer is present on the file, in the Selected insurer(s) dialog box, click on the desired insurer(s) to submit to. Click Ok.
.png?version=1&modificationDate=1407862200354&cacheVersion=1&api=v2)
- In the Submission complete confirmation box, click Ok.
In the Document successfully archived confirmation box, click Ok.
The HCFA form is automatically stored and assigned the 'Submitted' status in the patient's Documents tab.
Billing WSIB electronically (Canada only)
- After allocating a sale to WSIB, click the Tools drop-down menu, and select Electronic billing.
On the Unbilled invoices tab, click on the desired invoice, and click SUBMIT CLAIMS.
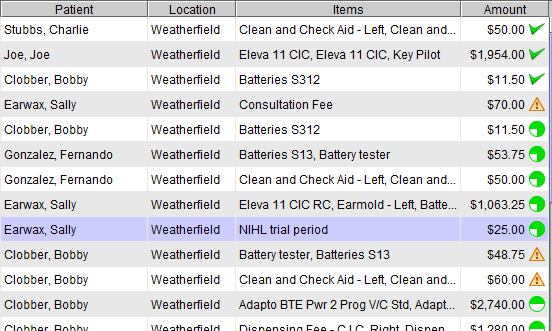
To submit multiple claims, press and hold the Control key (Ctrl) on the keyboard while clicking the desired invoices.Claims on the Unbilledinvoices tab with a triangle alert symbol contain one or more items that do not have correct WSIB coverage. Click on the submitted claim and click TRANSACTION DETAILS, or double-click the claim, to review the details. In the Review order screen, items without coverage are denoted with a triangle alert symbol. Edit the invoice, optionally adding coverage to the item(s), and then submit the claim.Click the Submitted claims tab to view submissions. The icon next to each claim represents the status. A quarter-green circle represents a claim which has just been submitted, and the various filled circles represent the different stages of the claim process. A green check mark indicates the submission is approved fully. An orange check mark indicates the submission was partially paid.
 Claims on the Submitted claims tab with a triangle alert symbol have been rejected. Verify the patient birth date and policy number accuracy. An Insurer Claim # is present for approved (and some denied claims). Contact WSIB, and provide the Insurer claim #, for additional information about the claim denial.
Claims on the Submitted claims tab with a triangle alert symbol have been rejected. Verify the patient birth date and policy number accuracy. An Insurer Claim # is present for approved (and some denied claims). Contact WSIB, and provide the Insurer claim #, for additional information about the claim denial.On the Submitted claims tab, optionally do any of the following:
Use the location drop-down menu to view one, or <All>, location(s).
- Optionally, click on a submitted claim and click CLAIM DETAILS to view claim items.
Optionally, click on a submitted claim and click CLEAR CLAIMS to remove it from the screen.
Ensure WSIB payments have been entered, prior to clearing the claim. Clearing a claim will remove the invoice from the Enter 3rd party payment screen.To clear multiple claims, press and hold the Control key (Ctrl) on the keyboard while clicking the desired invoices.
-
Page:
-
Page:
-
Page:
-
Page:
-
Page:
-
Page:
-
Page:
-
Page:
-
Page:
-
Page:
-
Page:
-
Page:
-
Page:
-
Page:
-
Page:
- No labels